Das Pilotprojekt von E-Rezepten in Polen ist für Februar geplant. Inwiefern ist die polnische Lösung mit denen in anderen Ländern vergleichbar? Ist das E-Rezept eine potentielle Bedrohung oder eine Chance für Apotheken? Wird es unabhängigen Apotheken Schaden bringen, die nicht über ausreichende Finanzmittel verfügen, um in Technologie und Marketing zu investieren? Wir haben uns die Erfahrungen im Bereich der E-Rezepte in Großbritannien, Estland und Deutschland angesehen.
E-Rezept in Großbritannien
Das britische Pharmaceutical Services Negotiating Committee (PSNC) fördert und unterstützt Anliegen von allen lokalen NHS-Apotheken ( Nationaler Gesundheitsdienst) in England. Wir haben PSNC um Kommentare zum Service von E-Rezepten in England gebeten, die im System The Electronic Prescription Service (EPS), 2. Auflage, abgewickelt werden.
Um das EPS-System zu verwenden, müssen Apotheken bestimmte Anforderungen erfüllen:
- Das PMR-System von medizinischer Patientendokumentation sollte vom Lieferanten des Apothekensystems geliefert werden.
- Es sollte Smart Cards für alle Mitarbeiter geben, die sich mit der Ausstellung von Rezepten befassen.
- Die Patienten sollten dem EPS-System zustimmen ( Nominierung).
Britische Apotheke

Quelle: inderApotheke
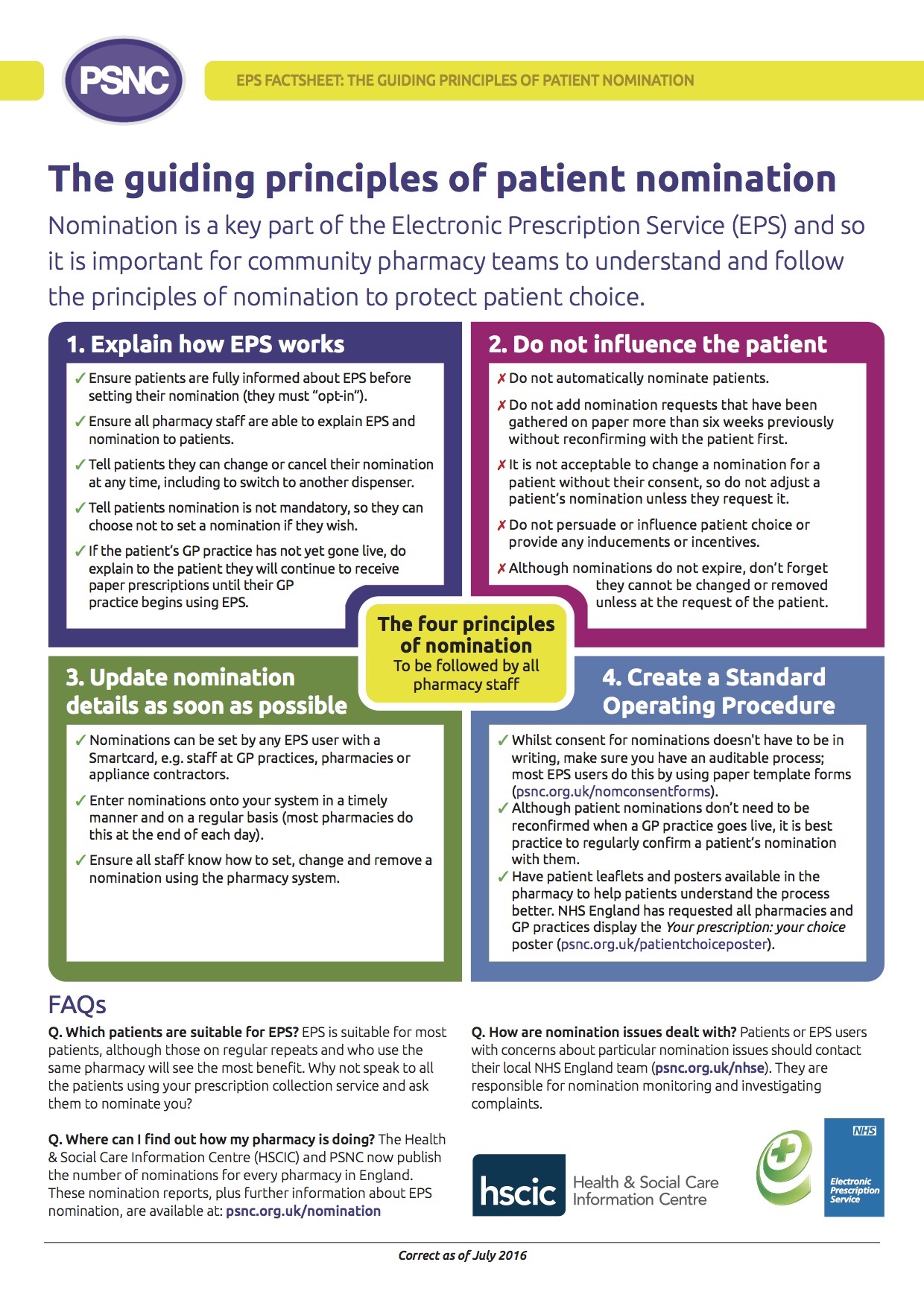
Was ist das Nominierungssystem?
In England verlangt derzeit EPS von Patienten, dass sie eine Apotheke benennen, die ihre elektronischen Rezepte erhalten wird. Um sicherzustellen, dass alle Arten von Apotheken – unabhängige, kleine oder Ketten - den EPS-Nominierungsregeln entsprechen, wurden Grundregeln für dieses Verfahren eingeführt.
Das Nominierungssystem kann zum Aufbau einer langfristigen Beziehung zwischen pharmazeutischen Teams und Patienten beitragen, weil die pharmazeutischen Teams Rezepte im Voraus erhalten und somit ist es möglich, Medikamente vorzubereiten, bevor der Patient in die Apotheke kommt, um sie abzuholen.
Allerdings zeichnet sich das System auch durch Flexibilität aus, weil diese EPS-Ernennung (Nominierung) auf Wunsch des Patienten vom beliebigen EPS-Benutzer (Person, die in der Apotheke oder in der Arztpraxis arbeitet) jederzeit geändert oder gelöscht werden kann. Es wird erwartet, dass eintägige Patienten ihre eigenen Nominierungseinstellungen auch anpassen könnten.
Quelle: PSNC
Wozu braucht man Papierrezepte?
Fast jede stationäre Apotheke hat die Funktion EPS, 2. Auflage eingeschaltet und kann somit EPS-Rezepte verarbeiten. Den neuesten Angaben vom NHS Business Services Authority( NHSBSA) kann man entnehmen, dass 23 Millionen aus den insgesamt 41 Millionen ausgestellten Rezepten, dem EPS-System gehören. Im September 2017 gab es daher circa 56% der E-Rezepte, und diese Zahl steigt.
Die Papierrezepte sind weiterhin für Medikamente erforderlich, die einer besonderen Kontrolle unterliegen (z.B. Morphin) oder, wenn der Patient beim NHS die Befreiung von Rezeptgebühren beantragen will. Doppelsysteme generieren nämlich zusätzliche Kosten und Belastungen für Apothekenmitarbeiter.
Papierrezept in England
Quelle: InDerApotheke
Herausforderungen für Apotheken in Großbritannien
Kollegen aus Großbritannien fassten die Herausforderungen hinsichtlich des EPS-Systems folgendermaßen zusammen:
- Das Volumen hängt natürlich von der Bereitschaft von Hausärzten ab, sich der elektronischen Rezepte zu bedienen, und bisher war ihr Engagement schwächer als im Fall der Apotheken.
- Es ergaben sich Fragestellungen in Bezug auf die Handlungskontinuität: wegen des Übergangs zu elektronischen Systemen, besteht ein Bedarf an der erhöhten Beständigkeit dieses Systems sowie an Notfallprozessen, wenn die Systeme versagen (z.B. Probleme mit Breitbandübermittlungen oder Stromausfällen).
- Notwendig sind angemessene Schulungen und Unterstützung für Ärzte, die Rezepte ausstellen und für das Personal, das dann Medikamente aushändigt.
- Kosten : sowohl für Apotheken, um Zugang zu den neuesten Systemaktualisierungen zu erhalten, als auch für Systemlieferanten, um ihre Systeme nach Erfüllung der Mindestanforderungen so nützlich wie möglich bereitzustellen.
- Das neue elektronische Modell benötigt immer noch Papier in einigen Fällen.
- Das aktuelle Smartcard -Modell/Technologie entspricht nicht der gängigen Arbeitsweise der meisten Apotheken. Jeder Mitarbeiter benötigt eine eigene Smartcard, um seine Identität zu bestätigen und um die Audit-Geschichte zur Verfügung stellen zu können. Das Einloggen braucht Zeit. In der Realität werden Apothekensysteme häufig von vielen Mitarbeitern verwendet, und viele Apotheken benutzen einen oder zwei Computer für alle Mitarbeiter, die Medikamente aushändigen.
E-Rezept in Estland
Wir haben Karin Alamaa-Aas, der Vorsitzenden der Pharmazeutischen Kammer in Estland, einige Fragen dazu gestellt, wie das E-Rezept in Estland funktioniert. Karin sagte, dass sowohl Ärzte als auch Apotheker mit dem elektronischen System zufrieden sind, weil es ein einfaches Tool ist, das die Papierrezepte vollkommen ausgeschlossen hat.
Patienten müssen nicht nur eine Apotheke anmelden - sie können dorthin gehen, wo sie Medikamente abholen wollen. Das Einzige, was vom Patienten benötigt wird, ist das Vorzeigen eigener ID-Karte in der Apotheke. Das Nominierungssystem existiert nicht, also gibt es keine Möglichkeit für dessen Missbrauch.
Wer waren die Gewinner und Verlierer?
In Apotheken in vielen Einkaufszentren und anderen populären Orten ist jetzt die Anzahl der Kunden gestiegen, weil Patienten nicht mehr zum Arzt gehen müssen, wenn sie ihre Rezepte erneuern wollen, sondern sie können das telefonisch machen. Die Situation verschlechterte sich im Fall der Apotheken in der Nähe des Hausarztes, weil sie aus diesem Grund einige Patienten verloren haben. Es besteht jedoch kein besonderes Risiko für unabhängige Apotheken, da die Funktionsweise des Systems keinen Gewinn größeren Akteuren bringt.
Aus der Sicht der Apotheker könnte allerdings das System weiter verbessert werden. Einer der Schwachpunkte ist der fehlende Zugang zu der medizinischen Dokumentation der Patienten, und es hindert daran, einen guten Ratschlag zu geben.
Obwohl das elektronische Rezept, trotz vieler Schwierigkeiten, in Estland und in Großbritannien endlich umgesetzt wurde, war der deutsche Versuch völlig erfolglos. Dies zeigt sehr deutlich, dass es einen kritischen Bedarf an der Berücksichtigung von Stimmen aller interessierten Parteien, darunter Apotheker und Ärzte gab.
Nachdem es sich ergab, dass die Zeit für die Ausstellung eines E-Rezepts fast doppelt so lange wie im Fall eines Papierrezepts ist, verweigerten die Ärzte, ein elektronisches Kartensystem zu bedienen, welches im nächsten Schritt rückgängig gemacht wurde.
Eine gute Übersicht über Fehler bei der Durchführung des Projekts wurde in der Arbeit zum Thema: Fehlgeschlagene Implementierung des E-Rezepts in Deutschland – Fallstudie ; Drews, Schirmer; 2015, präsentiert.
Zusammenfassend kann man Folgendes feststellen:
- Beim Projekt hat man sich auf technische Aspekte konzentriert, dabei wurden operatives Management und Change Management vernachlässigt.
- Allgemeine und integrierte Projektarchitektur wurde weder zu Beginn geliefert, noch im Laufe der Zeit entwickelt.
- Die Entscheidung, E-Gesundheit mit einem elektronischen Rezept zu beginnen, konnte aufgrund des Volumens (600 Millionen pro Jahr) und der Bedeutung dieses Prozesses fehlerhaft sein.
- Die Einwände seitens der Deutschen Ärzteversammlung wurden nicht ernst genommen; am Ende stimmten die Ärzte dafür, dass sich das System für die sichere Verarbeitung medizinischer Daten nicht eignet.
- Ärzte mussten mehr Zeit mit E-Rezepten verbringen (insgesamt 20 Minuten täglich), sie haben dennoch keine Vorteile des neuen Systems gesehen.
- Das Pilotprojekt, welches gleichzeitig in 7 Regionen in den Gang gesetzt wurde, war falsch konzipiert; Benutzer waren an mehreren Orten mit negativen Erfahrungen konfrontiert, die ihre Auswirkung in negativen Stimmungen hatten.
- Viele Fehler, die in dem Pilotprojekt ans Tageslicht kamen, hätte man genauso gut in früheren Tests auffinden können, wenn sie korrekt durchgeführt worden wären.
- Das Programm war unflexibel, mit begrenzten Möglichkeiten, Entscheidungen zu treffen. Es hat einige Jahre gedauert, bis man auf die aufgetretenen Schwierigkeiten reagierte.
- Die Analyse der Kosten und Nutzen wurde zu spät durchgeführt und nicht veröffentlicht. Leider zeigte sie nur Vorteile für Versicherungsgesellschaften, während Ärzte und Apotheken nur die Kosten untereinander teilten.
Fazit für E-Rezepte in Polen
Eine Besonderheit des polnischen Marktes ist der starke Wettbewerb zwischen großen Ketten und unabhängigen Apotheken. Das Nominierungssystem kann aus diesem Grund umstritten sein, weil es vorteilhaft für Kettenapotheken sein kann, die bereits in Beziehungen mit Lieferanten von medizinischen Dienstleistungen investieren, um für eigene Dienstleistungen zu werben. Allerdings werden Patienten in Polen das E-Rezept in beliebiger Apotheke wie in Estland einlösen können, so dass dieses Risiko vermieden wird.
Das E-Rezept kann ohne Unterstützung von Ärzten nicht wirklich umgesetzt werden.Wenn der gesamte Prozess zu schwierig oder zeitaufwendig ist, beispielsweise wegen Problemen mit der elektronischen Signatur, besteht die Gefahr, dass das System nicht akzeptiert werden wird. Andererseits scheint es, dass Apotheken neue Möglichkeiten ergreifen und ihre IT-Lieferanten mit notwendigen Funktionen ausgeröstet sind.
Pharmazeuten in Großbritannien betonen, dass Länder, die elektronische Systeme in Erwägung ziehen, ausreichende Geldmittel für Schulungen sowohl von Ärzten, die Rezepte ausstellen, als auch für pharmazeutische Teams, berücksichtigen sollten. In England sind Probleme aufgetreten, die dazu führten, dass Apotheken Gelder verloren, weil es Änderungen im Prozess gab, wie Rezepte zur Anrechnung und Kostenrückerstattung zu unterbreiten sind.
Wir sollten auch alle Gründe in Betracht ziehen, die zum Scheitern in Deutschland beitrugen, und über mögliche Lösungen von Problemen nachdenken. Warum ist das so wichtig? Die Antwort ist klar: langfristige Störungen kann sich das polnische Gesundheitssystem nicht leisten oder es braucht sie auch nicht.